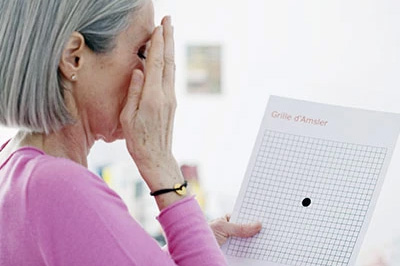
Age-Related Macular Degeneration
Macular degeneration is a progressive disease that affects the cells in the back part of your eye, which allows you to visualize objects that are straight ahead. Over time it damages your capacity for sharp, central vision. With macular degeneration, it becomes increasingly difficult to perform daily tasks such as reading or writing as well as recognizing faces or colors. Among the early signs of vision loss from macular degeneration, are shadowy areas in your central vision and unusually fuzzy or distorted vision. While individuals with advanced cases of macular degeneration are considered legally blind as the result of a profound loss of central vision, their peripheral vision, which is less clear than central vision, is retained. Most people do not experience vision loss in the early stage of age-related macular degeneration and the progression can be slow and painless.
An eye doctor can often detect early signs of macular degeneration before any symptoms are experienced. If signs of the condition are found, additional tests to verify the diagnosis may be ordered. Once the diagnosis has been confirmed, treatment to manage the condition and to slow the progression will be prescribed.
According to the National Eye Institute, over two million adults in the United States have age-related macular degeneration with that number expected to double within the next thirty years. While one defense against age-related vision loss is a nutritious diet and a healthy lifestyle, regular comprehensive eye exams are essential in order to protect the health of your eyes and the quality of your vision.
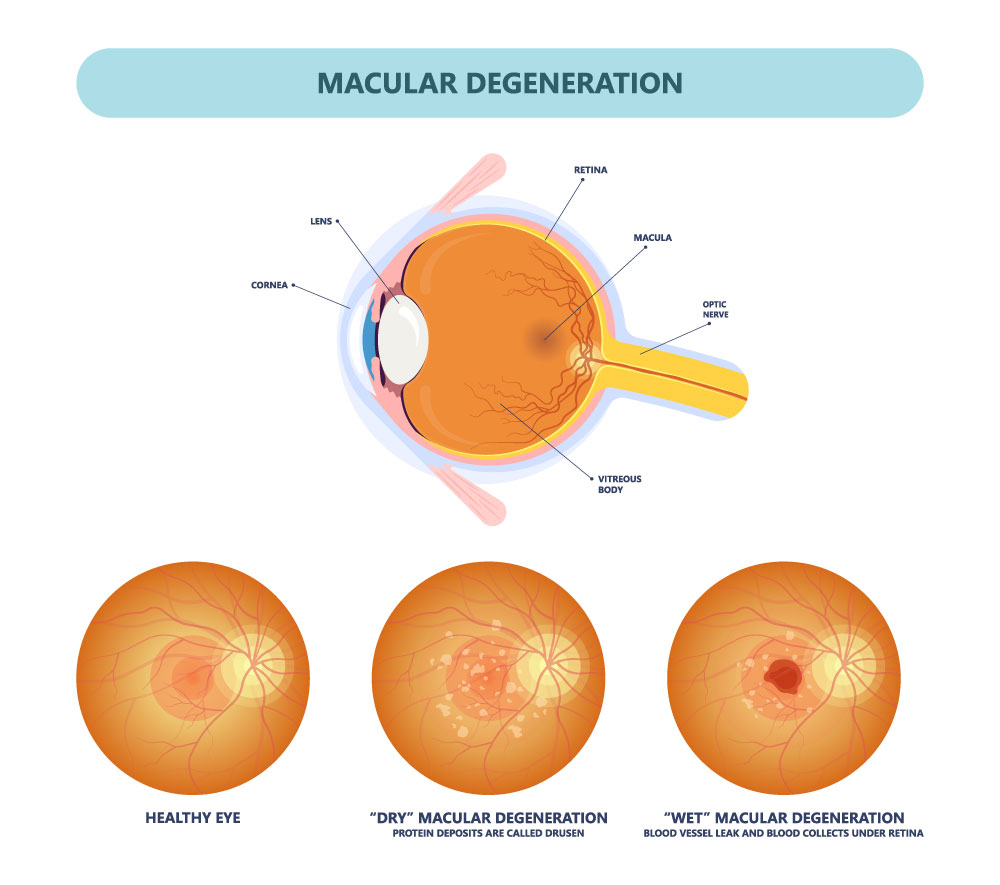
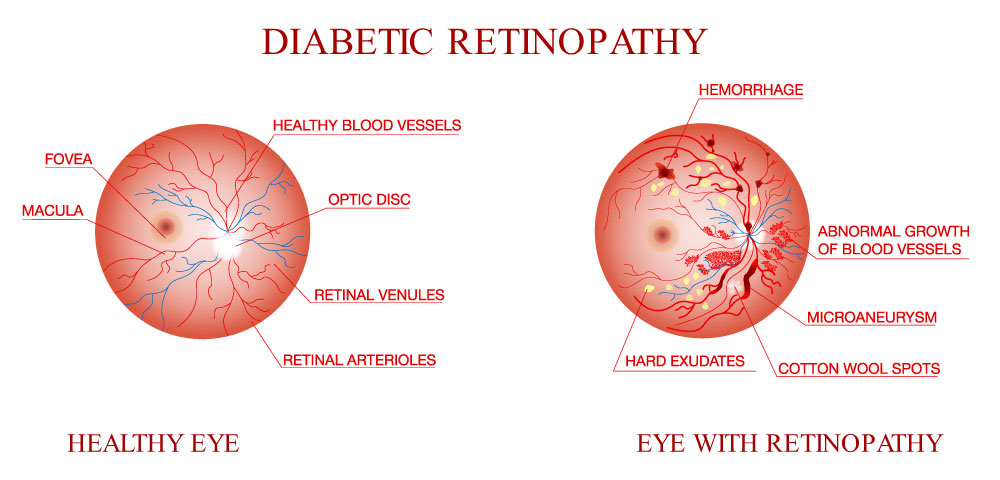
Diabetic Retinopathy
Diabetes is a complex metabolic disorder that impairs the body’s ability to produce or use insulin effectively to regulate blood sugar levels. Unfortunately, over time elevated blood sugar levels can cause damage throughout the body with many complications to one’s health and overall wellbeing. Diabetes contributes to the development of heart disease, stroke, kidney disease, eye problems, nerve impairment, and medical issues in the extremities.
The term “diabetic eye disease” refers to a group of conditions that potentially threaten the eyesight of people with diabetes.
This group of conditions includes:
- Diabetic Retinopathy
- Diabetic Macular Edema (DME)
- Cataracts
- Glaucoma
What is diabetic retinopathy?
The most common cause of vision loss among individuals with diabetes is diabetic retinopathy, which is a consequence of damage to the tiny blood vessels in the back of your eyes. While initially, you may not experience any symptoms, the complications of diabetic retinopathy can lead to severe vision problems and even blindness. Moreover, about half of those affected by diabetic retinopathy develop diabetic macular edema, which compromises the area of the retina used for reading, driving, and recognizing faces.
Background diabetic retinopathy, also known as non-proliferative diabetic retinopathy, offers an early, visible sign of small blood vessel disease. However, since the tiny aneurysms and hemorrhages that characterize this early stage may not produce noticeable vision changes, many diabetics remain unaware of an advancing disease process. Yet, once background diabetic retinopathy gets detected, it elevates the risk for more severe damage and vision loss,
Preventing vision loss
For people with diabetes, regular dilated eye exams are essential for early detection and the prevention of vision loss. In addition to scheduling a comprehensive dilated eye exam and controlling your blood sugar levels, it’s critical to pay close attention to any changes in your vision. Contact our office right away if you notice any sudden fluctuations or if your vision becomes spotty, blurry, or hazy.
Flashes and Floaters
Inside the orb-like structure of the eye, between the lens and the retina, is a large section known as the vitreous chamber. This chamber comprises 80% of the eye's structure and contains a clear fluid called the vitreous humour. This fluid performs several functions, including protecting the eye, helping to maintain its roundish shape, and keeping the retina in place. Although the vitreous humour, a gelatinous liquid, initially has a firm jelly-like consistency, the aging process can cause it to liquefy and shrink. When this happens, a few clumps of the vitreous humour may break away from the edges and start to float in the more liquid center. With entering light, these floating strands cast a shadow on the retina to create the appearance of drifting spots or threads.
What floaters look like
While floaters appearing as thread-like strands, cobweb-type shapes, or small shadowy dots can get very annoying, they are frequently benign and not a sign of retinal damage. However, in some cases, floaters and flashers indicate a more severe condition that can lead to vision loss.
According to statistics, about 70% of the population experiences a floater at some point in their lives. While you may not notice your floaters throughout the day, at various times, they may appear to drift aimlessly in front of your eye. They can be particularly annoying and noticeable when you are gazing at a blue or overcast sky or a computer screen with a white or light-colored background. Floaters appear to move as your eyes move and then dart away when you try to look at them directly.
Treatment
In many cases, floaters are no more than an accepted annoyance that one adapts to with time. However, when floaters impair vision, treatment may include surgery to remove and replace the vitreous with a solution that functions similarly or a laser procedure that may break up the floaters. It's also essential to address any underlying causes such as inflammation or bleeding from diabetes.
When to seek care
If you experience a sudden onset or abundance of floaters and spots, flashes of light in the same eye as your floaters, or notice peripheral vision loss, it's essential to get immediate care. Despite being painless, your eyesight may be in jeopardy.
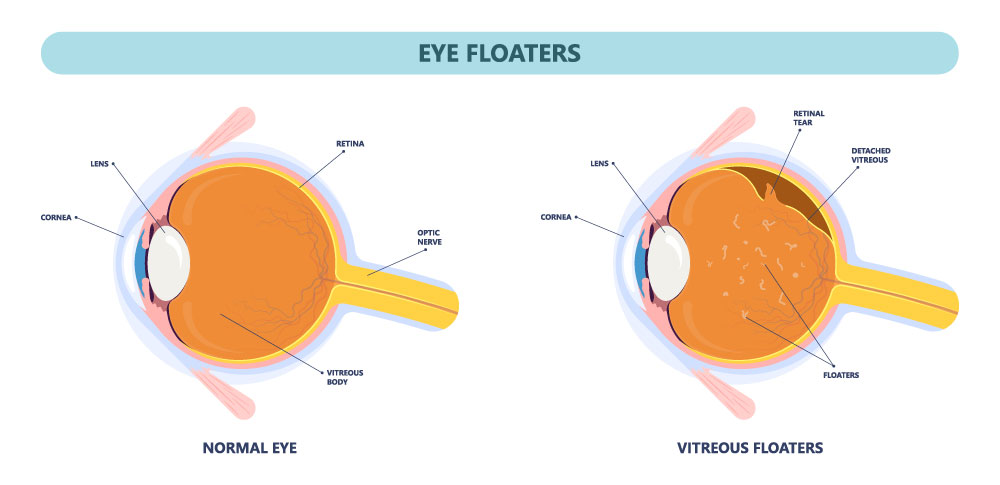
Retinal Tears
A retinal tear typically occurs with the aging process when the shrinking vitreous fluid in the eyeball causes the retina to tear instead of detaching from the underlying tissue in the back of the eye. While a torn retina can cause a range of vision changes, it can also lead to a retinal detachment with partial or complete vision loss.
The risk factors for a retinal tear closely resemble the risk factors for a retinal detachment, including:
- Advancing age
- Severe nearsightedness
- An eye injury
- Pre-existing eye conditions such as lattice degeneration
- Previous eye surgery
- Previous history of retinal tear
Signs and symptoms of a retinal tear
With a retinal tear, symptoms can include the sudden onset of floaters and flashes of light. An associated vitreous hemorrhage or retinal detachment can cause more severe symptoms such as blurred vision and the appearance of a curtain descending over a portion of the visual field.
Treatment
A retinal tear typically gets repaired during a surgical procedure. The good news is that with prompt care, the prognosis is good.The treatment for most retinal tears involves resealing the retina to the back wall of the eye with the use of laser surgery. These procedures create a scar that prevents leaking fluid from seeping under the retina and creating a worsening detachment.
It’s also worth noting that some retinal tears are asymptomatic and can resolve themselves. Low-risk retinal tears that fall into this category may get followed and observed without treatment.
Retinal Detachments
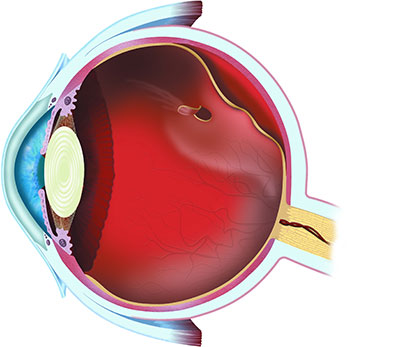
In the same way, a camera lens focuses the entering light on a piece of film to produce a sharp image, the lens of your eye focuses light on the retina to form a picture, which then gets sent to the brain.
Your retina acts in much the same way as the film in a conventional camera, with millions of photoreceptors known as rods and cones translating the focused light into full-color visual information.
A detached retina occurs when the light-sensitive tissue layer at the back of the eye gets pulled away from the underlying area. If not promptly treated, this situation can lead to permanent vision loss or blindness.
What causes a detached retina?
Although there are many reasons for a detached retina, most arise due to the aging process or an eye injury. Additional contributing factors include:
- Extreme nearsightedness or degenerative myopia
- Family history of retinal detachment
- Previous retinal detachment
- Eye surgery, including cataract surgery
- Diabetic retinopathy
- Lattice degeneration retinoschisis and other eye conditions
- Take glaucoma medications
Although it’s not always possible to prevent a retinal detachment, routine dilated exams can help find a minor tear or detachment before they impact one’s vision. Also, taking precautions like wearing protective eyewear can lower the risk of a contributing eye injury.
Being aware of the symptoms and getting prompt care
A retinal detachment can worsen quickly. For this reason, it’s essential to be mindful of any sudden onset vision changes, including:
- New floaters
- Blurred vision
- The sudden appearance of flashing lights
- Reduced peripheral vision
- Dark curtain appears in the visual field
Treatment
It’s imperative to get timely care to preserve eyesight as possible. Once diagnosed, surgical repair procedures may include a pneumatic retinopexy, scleral buckle, or vitrectomy. Results and improvement can vary, and healing can take quite some time.